Heart attack malpractice involves clots in arteries that cause muscle damage.
Misdiagnosis of heart attacks puts millions of patients at risk.
As many as 1.5 million people come to the hospital for "acute coronary syndrome." About 60,000 of those patients each year are sent home with detectable heart problems. For heart attacks, these involve blockages, which are like clogs in plumbing. Patients sent home with this blockage undiagnosed do not get the lifesaving heart treatment they need, because a careful and thorough process did not occur.
Chest pain can arise with heart problems. When the heart lacks oxygen for the muscle to work due to blockage, chest pain starts. That chest pain indicates muscle damage. But chest and abdomen pain have many other causes. So if chest pain is not evaluated with a careful, thorough process, misdiagnosis can kill a patient.
What is the best way to protect you and your loved ones? With unexpected, unpredictable chest pain after only moderate activity, the best thing to do is call an ambulance. While waiting, chew and swallow an aspirin, which will aid in clearing the plumbing problem.
When a heart attack attorney reviews a case, the attorney usually looks at two main issues:
Did a healthcare provider fail to diagnose a patient’s heart disease?
Before any lawsuit in Florida, a doctor must review the medical evidence to see whether there was a failure to diagnose.
For heart attack cases, diagnosis begins with a careful history. This history should explore the type of discomfort and its history.
This history can narrow the search. For instance, some pains exclude concern for heart problems. A sharp pain that gets worse with breathing is never heart related.
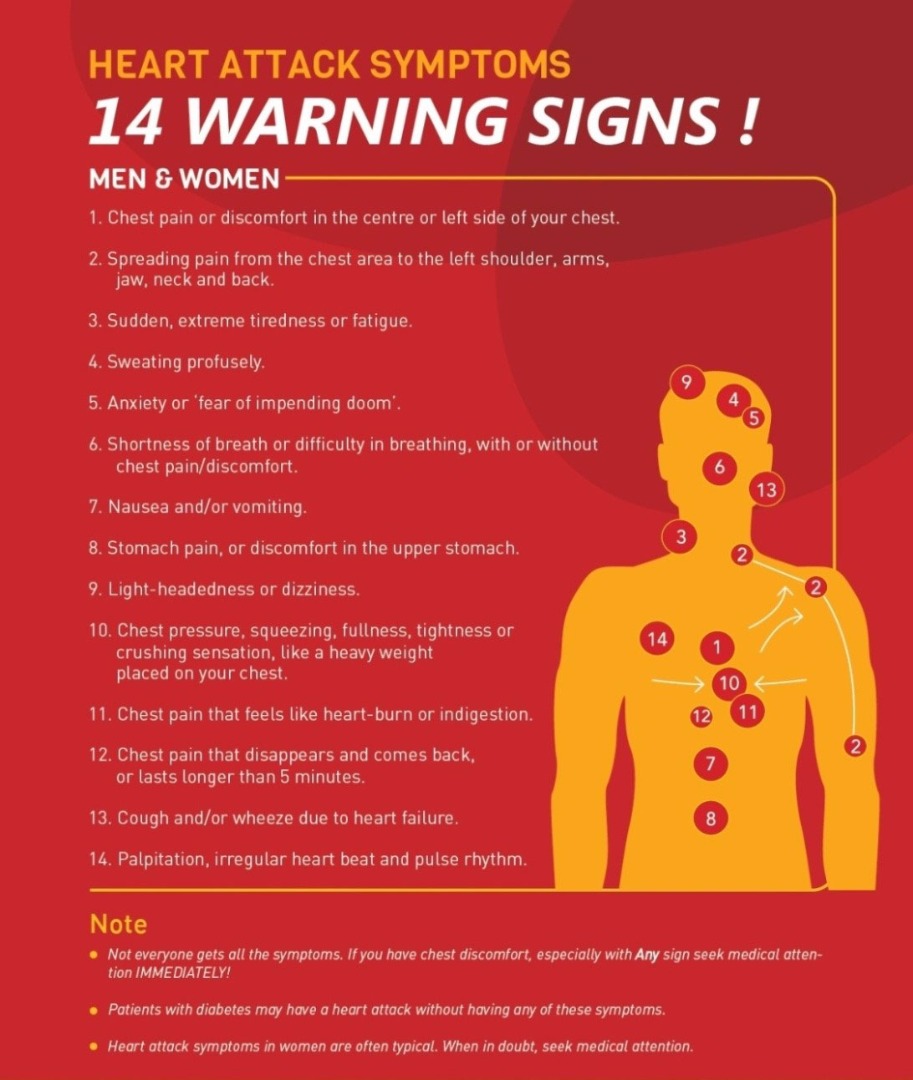
But many descriptions fit heart problems and require careful exploration. Chest pain in the center or left side of the chest is more suspicious of heart problems. A pain that spreads from the chest to the left shoulder, arms, jaw, neck, and back can indicate heart attack. Sudden and extreme fatigue can be a signal. So can sweating profusely, anxiety, shortness of breath, nausea, stomach pain, light-headedness, and palpitations. In short, patients can have a heart attack no report of chest pain, so careful follow up on reports of these other symptoms is necessary.
Reviewing the medical evidence, a reviewing doctor can determine whether the signs were there, and when a diagnosis should have been reached.
If so, would a doctor meeting the standard of care have reached the diagnosis in time to save the patient’s life?
A doctor must also determine the time for effective intervention. This time can range from hours before the attack, days before the attack, or even in the middle of the attack.
Once a heart attack is diagnosed, the hospital’s job is to get the patient into fast treatment. This treatment usually involves a balloon angioplasty to see if blocked arteries in the heart can be reopened before the heart muscle permanently dies. If a provider fails to move fast enough when the patient is having a heart attack, that provider has likely committed malpractice.
The common standards of care for heart attack patients are:
Angioplasty within 60 minutes, if possible, from the patient’s arrival at the emergency room.
If angioplasty is unavailable, clot-busting drugs (thrombolytics) as soon as possible, within 30 to 60 minutes of reaching the ER. These drugs chop up clots that already exist in the pipes. These drugs do not work if given after twelve hours from when heart attack symptoms begin.
Aspirin and Plavix for the heart on arrival and discharge. Unlike the clot-busting drugs, these drugs work because they stop platelets from sticking together. The absolute minimum standard is to give an aspirin within two hours of ER arrival (assuming you aren’t allergic) and then instruct the patient to take aspirin every day after the hospital stay.
Beta-blockers smooth out heart rhythm and slow the heartbeat. This protects the heart after a heart attack.
If a patient’s ejection fraction is under 40 percent at any time during a hospitalization, an ACE inhibitor drug should be prescribed at discharge. These drugs balance the heart’s reduced pumping efficiency by increasing the blood volume ejected by each heart beat and lowering the resistance of the tiny arteries in muscle, making it easier to get blood to the body.
The many warning signs of heart attack.
Tests for Heart Function That Can Indicate Heart Attack.
Heart studies, such as an EKG, echocardiogram, or a nuclear stress test are scientific ways to check the heart’s function.
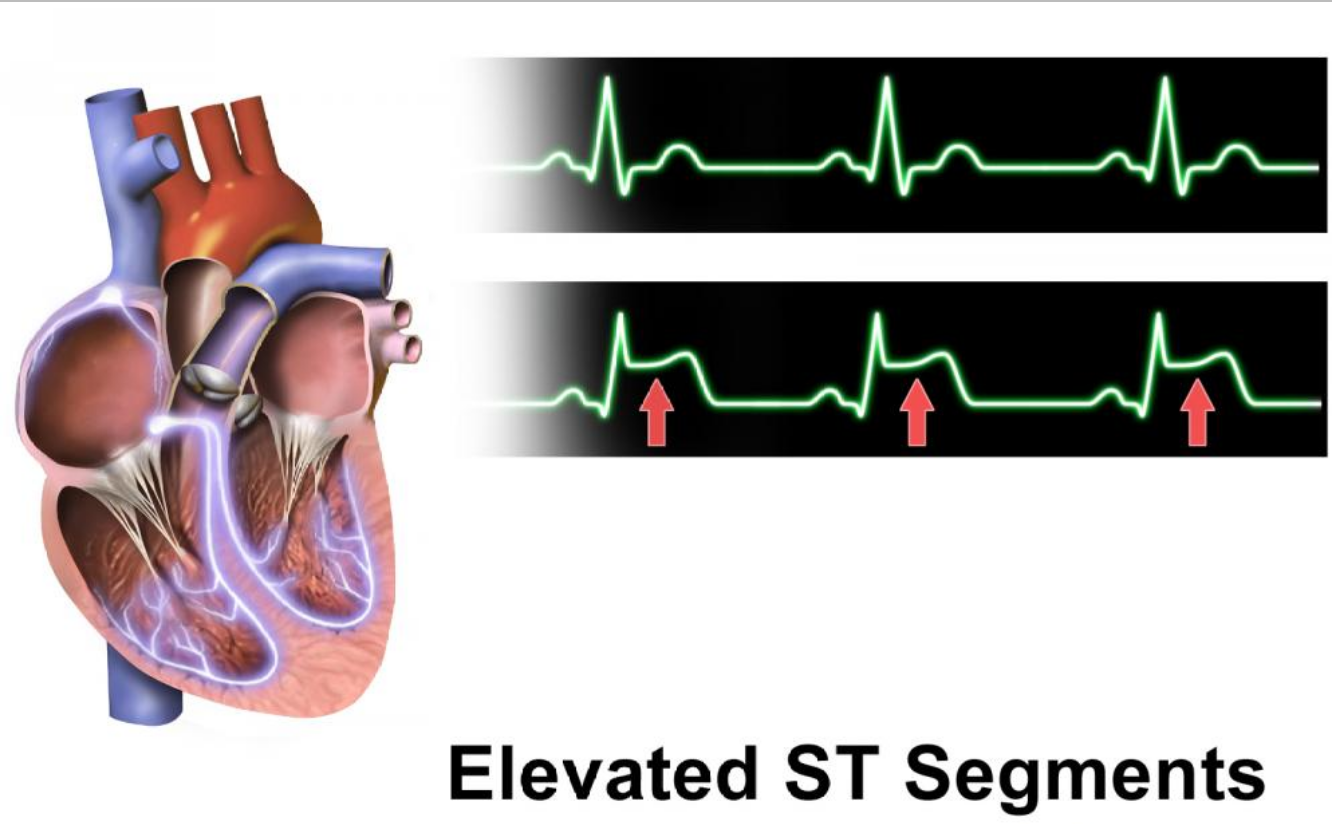
The EKG can tell you whether you have cardiac ischemia (too little blood to the heart) or whether you suffered a heart attack.
A single EKG does not rule out heart attack. EKG can be normal or non-diagnostic in up to 50% of patients who had a proven heart attack. So doing more than one EKG over a period of hours can be important if the diagnosis is not obvious.
If the EKG shows abnormal heart rhythm, other steps include echocardiogram and a nuclear stress test. These tests provide precise information about the heart’s function, such as your heart’s ability to pump blood (the “ejection fraction”).
Tests measuring cardiac enzymes also signal heart attack. Enzymes are proteins. Heart enzymes come from dying cells in the heart. The main ones tested for are troponin, creatinine phosphokinase (CK), and myoglobin. The most specific to the heart is troponin. Like a single EKG, a normal level of cardiac enzymes does not rule out heart attack. The testing could be too early, because enzymes don’t start to rise in the blood until three or more hours after harm to the heart. So the standard is to test cardiac enzymes at least twice, six hours apart, before confirming a “normal” result on the first lab was normal.
If an EKG shows blocked arteries leading to your heart or heart enzymes signal a heart attack, a cardiac catheterization can be done to confirm the blockage. A blockage of the arteries leading to your heart is the most common cause of heart attack. An operation to remove the plaque blocking your coronary artery can save your life.
Call me.
If you would like to discuss a potential legal matter or referral, call my office at 941-214-7122.